Monitor Unit (MU) is an essential parameter in radiation therapy that determines the amount of radiation to be delivered to the patient during treatment. The calculation of MU is a critical aspect of radiation therapy and must be performed accurately to ensure patient safety. There are several algorithms used to calculate MU, and one of the most precise and accurate methods is the Monte Carlo algorithm.
Monte Carlo algorithm in Radiation Therapy
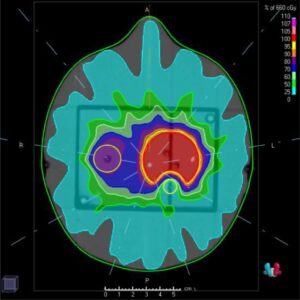
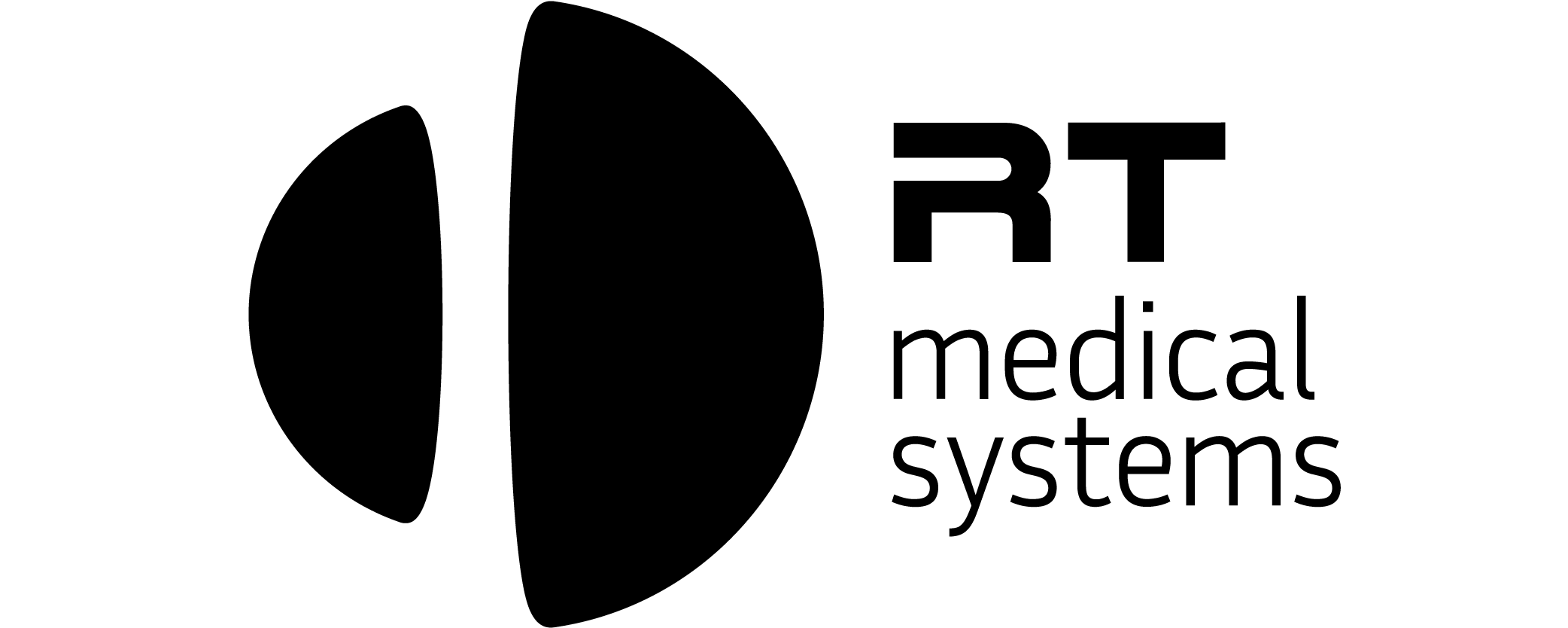
Isodose example
The Monte Carlo algorithm is based on computer simulations and uses statistical methods to calculate MU. The algorithm models the interactions of photons and electrons in a patient’s body and produces a dose distribution. This dose distribution is then used to determine the amount of radiation to be delivered to the patient.
The Monte Carlo algorithm offers several advantages over other algorithms used to calculate MU. The most significant advantage is its accuracy. The Monte Carlo algorithm takes into account the effects of scatter radiation, which can significantly impact the dose delivered to the patient. This algorithm is also highly versatile and can be used in complex treatment scenarios, such as when there are multiple radiation fields involved.
The Monte Carlo algorithm requires specialized software to perform the calculations. The software must be able to accurately model the interactions of photons and electrons in the patient’s body and must be able to handle large amounts of data. The software must also be able to produce accurate dose distributions that can be used to determine the amount of radiation to be delivered.
There are several steps involved in the calculation of MU using the Monte Carlo algorithm. The first step is to create a patient model that includes the patient’s anatomy and any relevant medical information. The next step is to define the treatment plan, including the radiation fields and the energy of the photons to be used. The Monte Carlo algorithm is then run to simulate the interactions of photons and electrons in the patient’s body and produce a dose distribution. The final step is to use the dose distribution to determine the amount of radiation to be delivered to the patient.
Dose calculation in the PTV
The Monte Carlo simulation for dose calculation in the PTV (Planning Target Volume) can be summarized in the following steps:
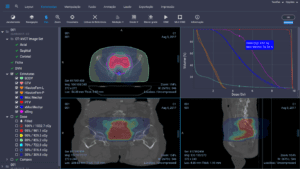
Secundary Check Software
Patient Model Creation: The first step is to create a detailed patient model that includes the patient’s anatomy, relevant medical information, and the location of the PTV.
Treatment Plan Definition: The next step is to define the treatment plan, including the energy of the photons to be used, the field size, and the number of fields.
Simulation Set-up: The Monte Carlo software must be set up to simulate the linear accelerator’s photon beam and the interactions of the photons and electrons in the patient’s body.
Photon Transport: The Monte Carlo algorithm simulates the transport of photons through the patient’s body, including the interactions of the photons with tissues and organs.
Dose Calculation: The Monte Carlo software calculates the dose delivered by the linear accelerator to the PTV based on the number of photons that reach the PTV and their energy.
Dose Verification: The final step is to verify the accuracy of the dose calculation by comparing it to measurements taken during actual treatment or with other dose calculation algorithms.
Adjustments: If necessary, the Monte Carlo simulation can be adjusted and re-run until the calculated dose matches the measured dose.
By following these steps, medical physicists can perform a Monte Carlo simulation to accurately calculate the dose delivered by a linear accelerator to a PTV inside the patient. This information is crucial for the safe and effective delivery of radiation therapy.
The Monte Carlo algorithm is an accurate and versatile method for calculating MU in radiation therapy. The use of specialized software is essential to perform the calculations and to produce accurate dose distributions. By using the Monte Carlo algorithm, medical physicists can ensure the safe and effective delivery of radiation therapy to their patients.